COVID-19: High Flow Nasal Cannula (HFNC)/Non-Invasive Positive Pressure Ventilation (NIPPV) Indications
| Summary /REVIEW of Recommendations of Universities and Societies
ICU Sept 2021 |
What are the thresholds for intubation and mechanical ventilation for patients who are not responding or deteriorating when on HFNC or NIPPV?
Summary of major recommendations
| Recommendation | Rating |
| If a patient with COVID-19 infection is not improving or is deteriorating under HFNC or NIPPV, then healthcare providers should have a low threshold for intubation and/or mechanical ventilation. | A |
| Use of HFNC may be indicated for COVID-19 patients with hypoxemic respiratory failure. | C |
| HFNC may be indicated over NIPPV as an initial course of treatment in COVID-19 hypoxemic respiratory failure when early intubation and ventilation is not indicated. | C |
| When HFNC is not available and intubation is not indicated, some recommendations suggest to consider a short NIPPV trial for COVID-19 hypoxemic respiratory failure. | C |
| BIPAP may be reserved for those with COVID-19 hypercapnic acute on chronic ventilatory failure – example COPD or OHS patient | C |
| CPAP may be indicated in COVID-19 patients with acute hypoxemic respiratory failure. | C |
Key: A–consistently recommended in multiple guidelines, B–recommended weak, C–guideline recommendations lacking or inconsistent data
Q1: Government guidelines on HFNC or NIPPV indications for COVID-19 patients
| Source | Recommendations |
| NHS | The use of NIPPV (BIPAP) should be reserved for those with hypercapnic acute on chronic ventilatory failure.
CPAP is the preferred form of NIPPV in the management of the hypoxemic COVID-19 patient (should not be used in those with agitation and confusion). Its use does not replace mechanical ventilation, but early application may provide a bridge to mechanical ventilation.. |
| CDC | The CDC refers care providers to guidelines put forth by the WHO as well as the Surviving Sepsis Campaign. |
| DoD
March |
HFNC is indicated over NIPPV when early intubation and ventilation is not possible, as it has shown to be both safer and more efficacious.
HFNC is indicated when oxygen therapy at 5-6 L/min is insufficient to maintain SpO2 92-96% and when invasive ventilation is unavailable. If HFNC is unsuccessful, early intubation is favored over BIPAP and other NIPPV. |
| WHO
March |
HFNC and NIPPV (including CPAP) are indicated only in select patients with hypoxemic respiratory failure.
HFNC: Potential contraindications for HFNC in COVID 19 patients are hypercapnia, hemodynamic instability, multiorgan failiure, or abnormal mental status, although emerging data suggest that HFNC may be safe in patients with mild-moderate and non-worsening hypercapnia. Attempt a short trial (1 hour) and intubate in case the patient acutely deteriorates or does not improve. NIPPV: Limited data suggest that NIPPV (CPAP or BiPAP) has a high failure rate in patients with viral infections |
Q1: Professional society statements on HFNC or NIPPV indications
| Source | Recommendations |
| ACCP | Use of HFNC in COVID-19 patients is controversial, and if necessary should only be utilized within an airborne infection isolation room.
Because it is known to be aerosol-generating, NIPPV [type not specified] is recommended against. Clinicians should instead consider early intubation. |
| SCCM/ ESICM |
HFNC: For adults with acute hypoxemic respiratory failure despite conventional oxygen therapy, SCCM suggests using HFNC over conventional oxygen therapy or NIPPV (Weak recommendation, low-quality evidence).
NIPPV: If HFNC is not available and there is no urgent indication for endotracheal intubation, SCCM suggests a trial of NIPPV with close monitoring and short-interval assessment for worsening of respiratory failure (Weak recommendation, low . |
| ASA | Due to limited efficacy, lack of airway protection, and risk of virus aerosolization, avoid NIPPV (CPAP or BiPAP) or HFNC in COVID-19 patients |
SCCM/ESCIM–Surviving Sepsis guidelines
Q1: Hospital guidance on HFNC or NIPPV indications
| Source | Recommendations |
| MGH | Where mechanical ventilation is available, it is the preferred means of respiratory support in COVID-19 patients. In the presence of bilateral infiltrates and hypoxemia, mechanical ventilation with low tidal volumes may be less injurious than continued vigorous spontaneous breathing with or without non-invasive support, but this benefit has to be weighed against the need for sedation often associated with mechanical ventilation..
NIPPV [BIPAP]: we should to continue to offer NIPPV in patients with hypercarbic respiratory failure and known COPD. |
| UCSF | HFNC can be considered in hypoxemic patients.
NIPPV (BiPAP and CPAP) may only be used in selected patients with respiratory failure |
Q2: Government guidelines regarding initiation of HFNC or NIPPV
| Source | Recommendations |
| NHS
April |
BIPAP suggested initial settings: PS 8-10 cm H20 + PEEP 5-10 cm H2O + 60% oxygen, targeting SpO2 88-92%.
CPAP suggested initial settings: 10 cm H2O + 60% oxygen. -MONITOR TV >9ml/kg. |
| CDC | CDC refers care providers to guidelines put forth by the WHO as well as the Surviving Sepsis Campaign. |
Government guidelines regarding thresholds for intubation and mechanical ventilation
| Source | Recommendations |
| NHS
April |
Recommendations strongly advocate early discussions seeking to ascertain ceilings of treatment at presentation in all patients, to avoid inappropriate escalation of ventilatory support. There should be a low threshold for intubation where there is clinical decline (which may include a rising oxygen requirement, consistently or rapidly declining SpO2, consistently or rapidly increasing respiratory rate and increased work of breathing). This should trigger immediate assessment for intubation and mechanical ventilation if deemed appropriate.
BiPAP: for those on BiPAP, excessive work of breathing is a possible indicator for intubation. CPAP Assess the response to CPAP within 30 minutes. If the patient responds, close observation and monitoring must continue for a further 6 hours to ensure no decline occurs, with careful monitoring continuing thereafter. Where there is no adequate response, where clinical decline continues, or where patient tolerance limits use, early intubation and mechanical ventilation should be sought where appropriate. Generally, aim for SpO2 92-96% or 88-92% for patients with chronic or acute on chronic type II respiratory failure. An SpO2 target of 90-93% is acceptable in patients with visible continuous pulse oximetry in an appropriately monitored environment. |
| CDC
April |
Surviving Sepsis Campaign. |
| DoD
March |
If HFNC is unsuccessful, early intubation is favored over BIPAP and other NIPPV. |
| WHO
March |
HFNC: intubate in case the patient acutely deteriorates or does not improve after a short trial (about 1 hour). |
Q3: Professional society statements regarding thresholds for intubation and mechanical ventilation
| Source | Recommendations |
| SCCM/ ESICM |
In adults with COVID-19 receiving NIPPV or HFNC, we recommend close monitoring for worsening of respiratory status, and early intubation in a controlled setting if worsening occurs (Best practice statement). |
SCCM/ESCIM–Surviving Sepsis guidelines
| UCSF | Patients who receive HFNC or NIPPV (CPAP or BiPAP) should be monitored hourly by staff capable of performing endotracheal tube intubation. Proceed directly to endotracheal intubation in patients with no evidence of improvement after short trials (e.g 1 hour). |
| MGH | Indications for intubation include increased work of breathing (accessory muscle use, tachypnea) and persistent or rapidly worsening hypoxemia. Note that some patients will deteriorate quickly. |
High flow nasal cannula.
NIPPV: Non-invasive Positive Pressure Ventilation. This designation may include bilevel positive airway pressure (BiPAP), continuous positive airway pressure (CPAP).
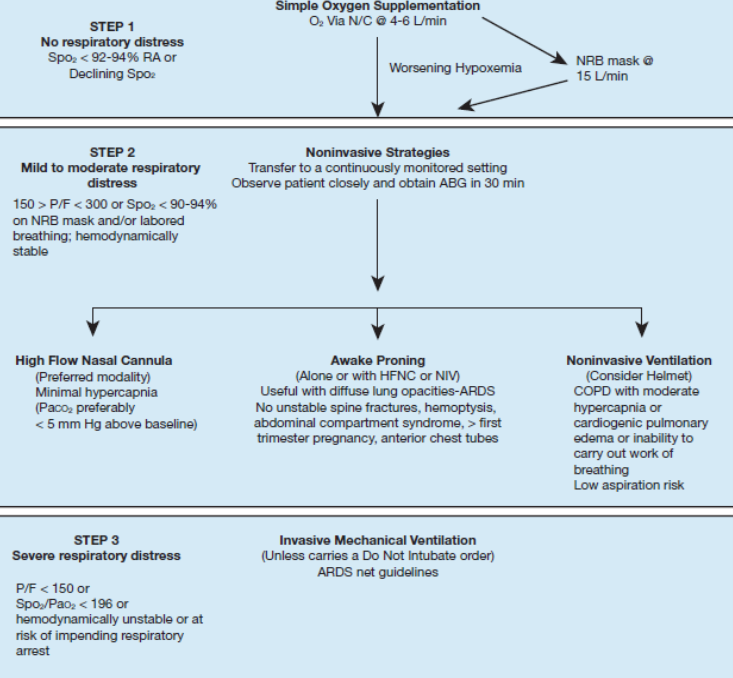
SUMMARY REC: Chest Review September 2020 –flow diagram
Authors:
- Nazir Habib, MD – Email: njhabib@med-specialists.net
- Christopher Voscopoulos, MD – Email: cjvoscopoulos@med-specialists.net
Copyright 2021 – Medical Specialists Associates