Effect of a Resuscitation Strategy Targeting Peripheral Perfusion Status vs Serum Lactate Levels
Monitoring patients with SEPTIC shock/ hypoperfusion in ICU patients is often complex and nebulous, and CMS guidelines currently recommend documentation by the MD and nurses, especially pertinent findings on physical examination including mental status (encephalopathy) and perfusion by capillary refill time ( CRT)/pulses etc.
Question arises whether these clinical finding are relevant or guide our resuscitation goals or outcomes in septic shock compared to checking LACTIC acid for clearance every 3-4 hours, which is based on clinical studies to be clinically useful and mandated by CMS.
INTERVENTIONS:
Patients were randomized to a step-by-step resuscitation protocol aimed at either normalizing capillary refill time (n = 212) or normalizing or decreasing lactate levels at rates greater than 20% per 2 hours (n = 212), during an 8-hour intervention period.
MAIN OUTCOMES AND MEASURES:
The primary outcome was all-cause mortality at 28 days.Secondary outcomes were organ dysfunction at 72 hours after randomization, as assessed by Sequential Organ Failure Assessment (SOFA) score (range, 0 [best] to 24 [worst]); death within 90 days; mechanical ventilation–, renal replacement therapy–, and vasopressor-free days within 28 days; intensive care unit and hospital length of stay.
RESULTS:
Among 424 patients randomized (mean age, 63 years; 226 [53%] women),416 (98%) completed the trial. By day 28, 74 patients (34.9%) in the peripheral perfusion group and 92 patients (43.4%) in the lactate group had died (hazard ratio, 0.75 [95%CI,0.55 to 1.02]; P = .06; risk difference, −8.5%[95%CI, −18.2%to 1.2%]). Peripheral perfusion–targeted resuscitation was associated with less organ dysfunction at 72 hours (mean SOFA score, 5.6 [SD, 4.3] vs 6.6 [SD, 4.7]; mean difference, −1.00 [95%CI, −1.97 to −0.02]; P = .045). There were no significant differences in the other 6 secondary outcomes. No protocol-related serious adverse reactions were confirmed.
CONCLUSIONS AND RELEVANCE:
Among patients with septic shock, a resuscitation strategy targeting normalization of capillary refill time, compared with a strategy targeting serum lactate levels, did not reduce all-cause 28-day mortality. However organ dysfunction was LOWER in CRT group
COMMENTS;
This is very useful study for all clinicians who follow clinical findings such as encephalopathy, mottling and delayed CRT at the bedside while waiting for lactic acid levels to be drawn.
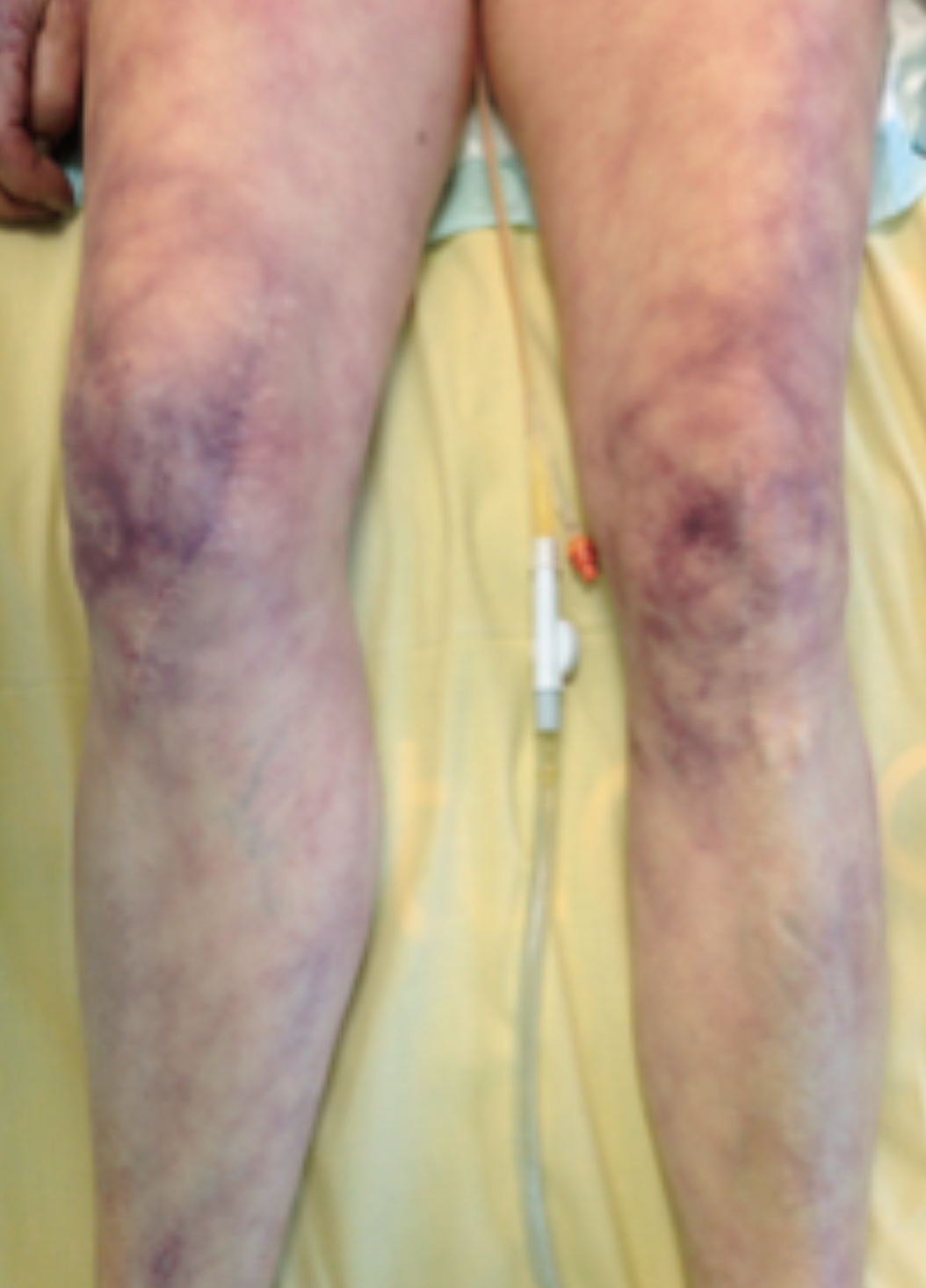
In addition to always evaluating fluid responsiveness in ALL patients as recommended by CMS, this study did show the utility of paying attention to CRT as a sign of poor perfusion (mottled/cold extremities) and, perhaps inadequate resuscitation, as all the secondary outcome in the CRT groups were either better ( organ dysfunction) or no worse.
In the end shock presents with a constellation of physical signs, and poor peripheral perfusion, resulting in target organ damage and evaluating patients with mottling or delayed CRT is a useful clinical parameter.
750 patients in ICU with mottled knees = Mortality increased 4 fold & if Lactic is over 2, mortality increased 5 Fold!! If patient remains mottled after 6 hour bundle=MORTALITY is over 40%
Great nurse information to share
For another interesting article on peripheral perfusion, check out this:
Intensive Care Med 2015:41: 452: Coudroy
Dr. Habib Nazir
ICU Lodi AH Director
Professor Critical Care CNSU Medical School
This was a study from Chile that was presented at SCCM in San Diego: JAMA. 2019;321(7):654-664:Hernadez


